In the United States, the rate of fetal death in utero after 20 weeks, known as stillbirth or stillbirth in English, is back on the rise, reaching 5.7 per 1,000 births and more than 10 per 1,000 among African American women.
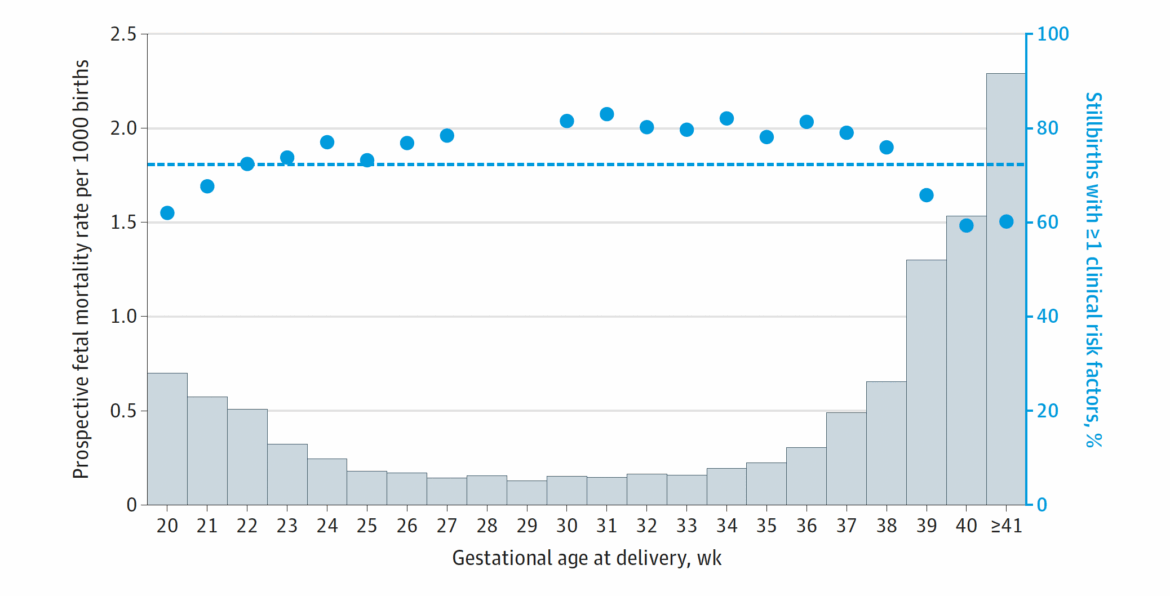
A large prospective study published in JAMA in 2025, conducted on nearly 3 million pregnancies between 2016 and 2022, reveals this.
Being a prospective study based on clinical data, and not as often on administrative records or death certificates, this work is particularly reliable and sensitive: it takes a more accurate picture of the reality of fetal loss and shows a phenomenon that is far from resolved.
The authors estimate that about half of fetal deaths at term could be prevented by better obstetric surveillance, regular checkups and more equitable care of pregnant women.
But they also recall that one-third of fetal deaths occur in the absence of recognized risk factors, confirming how important it is to maintain an active system of care that leaves no one behind, even pregnancies considered “low-risk.”
Even in high-income countries, we cannot let our guard down
This research reinforces the reflections we presented in the international paper published in BMC Pregnancy and Childbirth in 2023(de Graaff et al., with participation from CiaoLapo and the University of Florence).
This study created the first “International Scorecard” for high- and middle-income countries, a system of indicators to measure progress in birthbirth prevention and quality of bereavement care.
The results leave no room for doubt:
-
strong inequalities exist between and within countries, with rates ranging from 2‰ in Finland to 7‰ in Brazil, and with higher values in socially, ethnically or geographically disadvantaged groups;
-
most countries have no national goals or plans to reduce stillbirth, and few (only 3 of 13) have guidelines for perinatal bereavement care;
-
data collection is patchy and often lacks indicators of equity and quality of care, making it difficult to truly assess where and why more people are dying;
-
Finally, only one in three countries have national strategies in place to combat stigma and improve public awareness of an issue that is still too invisible.
These shortcomings make it clear that, even in advanced health systems, progress is never guaranteed: without targeted public policies, birth-mortality rates may stop falling, or even rise again.
And in Italy? Good results, but be careful not to let your guard down
We know that in our country the birth rate is among the lowest in Europe, but we cannot afford to consider it an acquired success.
The positive average level hides important territorial differences and signs of fragility in pregnancy care pathways.
In recent years, some areas have seen reductions in universal access to basic services, rarer or delayed obstetrical visits, staff shortages, and a gradual weakening of the territorial maternity support network, especially in rural and disadvantaged settings.
These phenomena, if not addressed, can increase the risk of fetal loss, especially among women who already start from more vulnerable health or living conditions.
For this reason, it is essential that Italy maintains and strengthens the Essential Levels of Care (LEAs), truly guaranteeing all women, regardless of income, citizenship or place of residence, continuous, free and quality access to monitoring and prevention services in pregnancy.
Maternal and fetal health protection is a fundamental right, and LEAs must ensure universal coverage: regular obstetric visits, appropriate diagnostic tests, multidisciplinary care in case of complications, and an integrated network between territory and hospital.
This is the only way to prevent prevent preventable deaths and promote true perinatal health equity, a goal that the World Health Organization itself lists as a global priority to be achieved by 2030.
Main references
-
Sullivan et al, Stillbirths in the United States, JAMA 2025 – https://jamanetwork.com/journals/jama/fullarticle/2840578
-
de Graaff et al, Ending Preventable Stillbirths and Improving Bereavement Care, BMC Pregnancy and Childbirth 2023 – https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-05765-5